Erisipela, a skin infection caused by bacteria, is not your average skin irritation. It’s a fiery invader that sets the skin ablaze, leaving behind a trail of redness, swelling, and discomfort. Join us as we delve into the fascinating world of Erisipela, exploring its causes, symptoms, treatments, and preventive measures. Get ready for an interactive journey that will leave you armed with knowledge and ready to conquer this skin adversary!
Definition and Overview of Erysipelas
Erysipelas is a superficial bacterial infection of the skin that typically affects the face, legs, or arms. It is caused by bacteria, most commonly Streptococcus pyogenes (group A streptococcus), which enter the skin through a break in the skin, such as a cut, abrasion, or insect bite.
Clinical Presentation
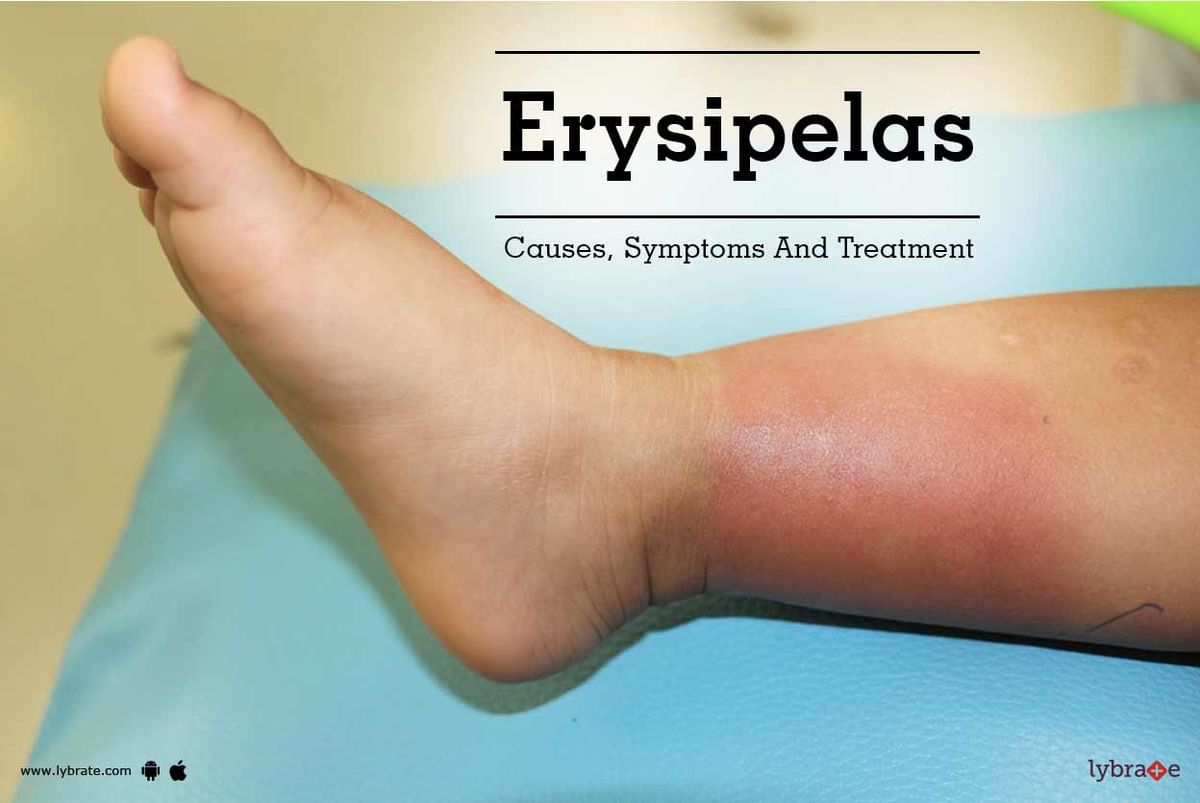
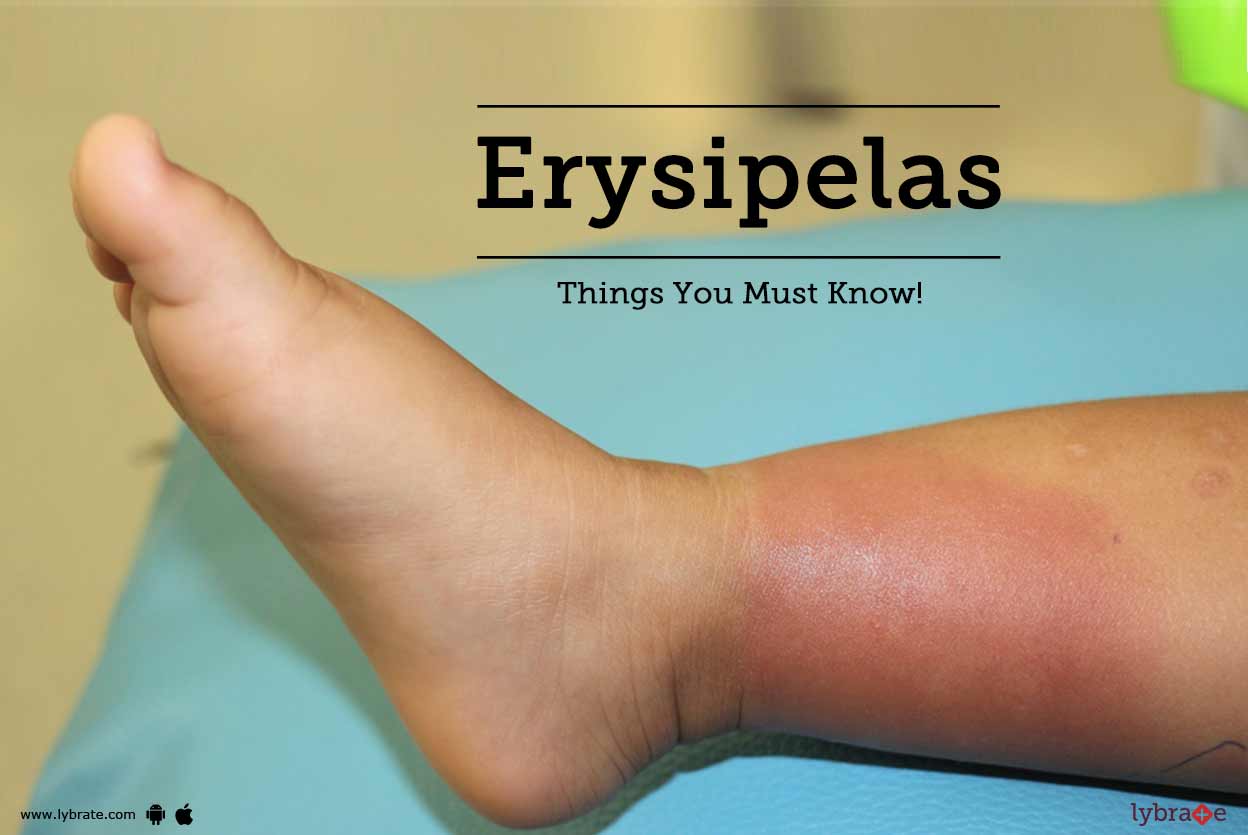
Erysipelas typically presents with a red, swollen, and tender area of skin that is warm to the touch. The affected area may also be painful and have a burning or itching sensation. In severe cases, the infection can spread to the underlying tissues, causing cellulitis or abscesses.
Causes and Risk Factors: Erisipela
Erysipelas is primarily caused by a bacterial infection, most commonly by Streptococcus pyogenes, also known as Group A streptococcus (GAS).
Certain factors increase the risk of developing erysipelas, including:
Predisposing Conditions
- Lymphedema: A condition that causes fluid buildup in tissues, often in the legs or arms.
- Leg ulcers: Open sores on the legs that can become infected.
- Diabetes: A chronic condition that impairs the body’s ability to heal wounds.
- Obesity: Excess weight can put pressure on lymphatic vessels, increasing the risk of fluid buildup and infection.
Other Risk Factors
- Skin breaks or wounds: Any break in the skin can provide an entry point for bacteria.
- Poor hygiene: Inadequate hygiene practices can increase the risk of skin infections.
- Weakened immune system: Individuals with weakened immune systems are more susceptible to infections.
- Insect bites or animal scratches: Bites or scratches can introduce bacteria into the skin.
Pathophysiology and Progression
Erysipelas is a bacterial infection that affects the superficial layers of the skin and the underlying lymphatic channels. The pathophysiology of erysipelas involves the invasion of bacteria, typically Streptococcus pyogenes or Staphylococcus aureus, into the skin through breaks in the skin’s barrier, such as cuts or abrasions. Once the bacteria enter the skin, they multiply and spread rapidly through the lymphatic channels, causing inflammation and swelling.
Initial Stage
The initial stage of erysipelas is characterized by the development of a localized area of redness, warmth, and swelling on the skin. The affected area is often well-demarcated and has a raised, sharply defined border. The skin may also become tense and shiny, and the patient may experience pain and tenderness.
Progressive Stage
As the infection progresses, the bacteria continue to spread through the lymphatic channels and deeper layers of the skin. This can lead to the formation of bullae (fluid-filled blisters) and vesicles (small, raised, fluid-filled sacs). The affected area may also become more extensive and the skin may become discolored.
Advanced Stage
In severe cases, erysipelas can lead to systemic complications, such as sepsis. Sepsis is a life-threatening condition that occurs when bacteria enter the bloodstream and spread throughout the body. Risk factors for severe erysipelas include diabetes, obesity, and a weakened immune system.
Differential Diagnosis

Differentiating erysipelas from other skin infections is crucial for appropriate treatment and management. Key features that distinguish erysipelas include its characteristic raised, well-demarcated, and erythematous borders, along with the presence of lymphedema and systemic symptoms like fever and chills.
Comparative Clinical Features
The table below compares the clinical features of erysipelas with those of other common skin infections:
| Characteristic | Erysipelas | Cellulitis | Impetigo | Stasis Dermatitis |
|---|---|---|---|---|
| Borders | Raised, well-demarcated | Indistinct | Sharply demarcated | Irregular |
| Erythema | Bright red | Pink or red | Yellow or honey-colored crusts | Dark red or purple |
| Edema | Present | May be present | Absent | Present |
| Lymphedema | Common | Uncommon | Absent | Present |
| Systemic symptoms | Fever, chills, malaise | May be present | Absent | Absent |
| Underlying cause | Streptococcal infection | Bacterial infection | Staphylococcal or streptococcal infection | Venous insufficiency |
Note: The presence of lymphedema and systemic symptoms are key differentiating features of erysipelas.
Images
Erysipelas:
Cellulitis:
Impetigo:
Stasis Dermatitis:
Diagnostic Tests and Procedures
Confirming erysipelas requires a combination of clinical examination and diagnostic tests. These tests aim to identify the presence of bacterial infection, rule out other conditions, and guide treatment decisions.
The choice of diagnostic tests depends on the severity of the infection, the patient’s overall health, and the availability of resources.
Skin Biopsy
A skin biopsy involves removing a small sample of the affected skin for examination under a microscope. This test can confirm the presence of bacteria and rule out other skin conditions with similar symptoms.
Culture
A culture involves collecting a sample of fluid or tissue from the affected area and growing it in a laboratory to identify the specific bacteria causing the infection.
Imaging
Imaging tests, such as ultrasound or MRI, may be used to assess the extent of the infection and rule out underlying complications like abscess formation.
Differential Diagnosis
Erysipelas shares similar symptoms with other skin infections and conditions. Differential diagnosis is crucial to rule out these conditions and ensure appropriate treatment.
Common Differential Diagnoses
- Cellulitis
- Necrotizing fasciitis
- Lymphangitis
- Deep vein thrombosis (DVT)
- Stasis dermatitis
Treatment Options
The primary treatment for erysipelas is antibiotics. The choice of antibiotic and the duration of therapy depend on the severity of the infection.
For mild cases of erysipelas, oral antibiotics such as penicillin or erythromycin are usually effective. For more severe cases, intravenous antibiotics such as vancomycin or clindamycin may be necessary.
Duration and Dosage of Antibiotic Therapy
The duration of antibiotic therapy for erysipelas typically ranges from 7 to 10 days. The dosage of the antibiotic will depend on the type of antibiotic being used and the severity of the infection.
Surgical Debridement
Surgical debridement may be necessary in some cases of erysipelas, such as when there is a large area of skin involvement or when the infection is not responding to antibiotic therapy.
Indications for Hospitalization
Hospitalization may be necessary for patients with severe erysipelas, such as those who have a high fever, chills, or other systemic symptoms.
Adjunctive Therapies
Adjunctive therapies, such as elevation and compression, can help to reduce swelling and pain in erysipelas.
Prevention and Recurrence
Erysipelas can be a recurrent infection, but there are steps you can take to prevent it from coming back.
Hygiene and Wound Care
- Wash your hands frequently with soap and water, especially after touching anything that may have bacteria on it.
- Keep your skin clean and dry, especially if you have any cuts or scrapes.
- Cover any open wounds with a clean bandage to prevent bacteria from entering.
Risk Factors for Recurrence
There are certain factors that can increase your risk of developing erysipelas again, including:
- Having an underlying medical condition that weakens your immune system, such as diabetes or kidney disease.
- Having lymphedema, which is a condition that causes swelling in your arms or legs.
- Poor hygiene practices.
Strategies for Reducing Recurrence Risk
- Manage any underlying medical conditions that may weaken your immune system.
- Control lymphedema by elevating your affected limb and wearing compression stockings.
- Improve your hygiene practices by washing your hands frequently, keeping your skin clean and dry, and covering any open wounds.
Prevention and Recurrence Measures
| Measure | Description | Rationale |
|---|---|---|
| Hand hygiene | Wash hands frequently with soap and water, especially after touching anything that may have bacteria on it. | To prevent the spread of bacteria to the skin. |
| Skin care | Keep skin clean and dry, especially if you have any cuts or scrapes. | To prevent bacteria from entering the skin. |
| Wound management | Cover any open wounds with a clean bandage to prevent bacteria from entering. | To prevent infection. |
| Management of underlying medical conditions | Manage any underlying medical conditions that may weaken the immune system. | To reduce the risk of infection. |
| Control of lymphedema | Control lymphedema by elevating your affected limb and wearing compression stockings. | To reduce the risk of infection. |
| Improvement of hygiene practices | Improve your hygiene practices by washing your hands frequently, keeping your skin clean and dry, and covering any open wounds. | To prevent the spread of bacteria. |
Complications and Prognosis
Erysipelas can lead to serious complications if left untreated.
Potential complications include:
- Cellulitis: Infection of the deeper layers of the skin.
- Abscess formation: Collection of pus beneath the skin.
- Lymphangitis: Infection of the lymphatic vessels.
- Necrosis: Death of skin tissue.
- Sepsis: Life-threatening infection of the bloodstream.
With prompt treatment, most cases of erysipelas resolve within 7-10 days. However, in severe cases, recovery may take several weeks or months. Recurrence is possible, especially in individuals with underlying health conditions.
Epidemiology and Public Health
Erysipelas is a common bacterial skin infection that primarily affects the lower extremities. Its epidemiology varies geographically, with higher incidence rates reported in certain regions. Understanding the prevalence and incidence of erysipelas is crucial for public health planning and surveillance.
Prevalence and Incidence
- The global prevalence of erysipelas is estimated to be around 0.5-1.5 cases per 1000 population per year.
- Incidence rates vary significantly by region, with higher rates observed in tropical and subtropical areas.
- In the United States, the incidence of erysipelas is estimated to be approximately 0.2-0.5 cases per 1000 population per year.
- Erysipelas is more common in older adults, with the highest incidence rates occurring in those over the age of 65.
Public Health Implications
Erysipelas poses significant public health concerns due to its potential complications and impact on healthcare resources. The infection can lead to severe complications, including cellulitis, lymphedema, and sepsis. Additionally, erysipelas can result in prolonged hospitalization and substantial healthcare costs.
Surveillance
Surveillance of erysipelas is important for monitoring disease trends, identifying risk factors, and implementing appropriate public health interventions. Currently, erysipelas is not a nationally notifiable disease in most countries, which limits the availability of comprehensive surveillance data.
Limitations of Current Surveillance System
The current surveillance system for erysipelas has several limitations:
- Incomplete reporting: Erysipelas is often underreported due to its non-specific symptoms and the lack of mandatory reporting requirements.
- Lack of standardized case definition: The absence of a standardized case definition makes it difficult to compare data across different regions and time periods.
- Limited data on risk factors: Surveillance systems often lack detailed information on risk factors, making it challenging to identify vulnerable populations.
Improvements to Surveillance System
To improve the surveillance of erysipelas, several measures can be implemented:
- Increase reporting: Encourage healthcare providers to report all suspected cases of erysipelas to public health authorities.
- Establish a standardized case definition: Develop a clear and consistent case definition to ensure accurate and comparable data collection.
- Collect detailed data: Enhance surveillance systems to capture information on risk factors, clinical characteristics, and outcomes of erysipelas cases.
- Use electronic health records: Utilize electronic health records to facilitate data collection and improve the completeness and timeliness of reporting.
Case Studies and Clinical Examples
Erysipelas is a common skin infection caused by Streptococcus pyogenes. It is characterized by a red, swollen, and painful area of skin that typically occurs on the lower legs. Erysipelas can be treated with antibiotics, but it can be a serious infection if not treated promptly.
Clinical Examples
- A 65-year-old woman presents with a red, swollen, and painful area on her right lower leg. She has a history of diabetes and has had several previous episodes of erysipelas.
- A 40-year-old man presents with a red, swollen, and painful area on his left lower leg. He has no history of diabetes or other medical conditions.
- A 25-year-old woman presents with a red, swollen, and painful area on her right arm. She has a history of eczema and has had several previous episodes of cellulitis.
In each of these cases, the patient was diagnosed with erysipelas based on the clinical presentation and history. All three patients were treated with antibiotics and recovered without any complications.
Illustrations and Images
Erysipelas is a bacterial skin infection characterized by a distinctive reddish, raised, and swollen appearance. To better understand the clinical presentation of erysipelas, we have compiled a gallery of high-quality illustrations and images.
Each image is accompanied by a detailed description and caption, providing valuable insights into the typical features of erysipelas and its progression.
Image Gallery
- Image 1: Early Stage Erysipelas
This image depicts the early stage of erysipelas, showing a localized area of redness, swelling, and tenderness on the skin.
- Image 2: Progression of Erysipelas
This image demonstrates the progression of erysipelas, with the redness and swelling spreading rapidly across the skin, forming a raised, well-demarcated border.
Find out about how Miranda Sarmento can deliver the best answers for your issues.
- Image 3: Severe Erysipelas
This image illustrates a severe case of erysipelas, characterized by extensive redness, swelling, and blistering, involving a large area of skin.
- Image 4: Erysipelas on the Face
This image shows erysipelas affecting the face, causing significant swelling and redness around the eyes and cheeks.
- Image 5: Erysipelas on the Leg
This image depicts erysipelas on the leg, demonstrating the typical raised, reddish appearance and involvement of the lower extremity.
Research and Advancements
Erysipelas research continues to make strides in understanding and treating this bacterial infection. Researchers are actively exploring novel diagnostic techniques, antimicrobial agents, immunotherapies, and surgical interventions to improve patient outcomes.
These advancements have the potential to reduce morbidity and mortality, improve quality of life, and enhance cost-effectiveness in erysipelas management.
Browse the implementation of KV Kortrijk in real-world situations to understand its applications.
Novel Diagnostic Techniques
- Molecular diagnostics, such as PCR and multiplex assays, offer rapid and sensitive detection of Erysipelothrix rhusiopathiae, the causative agent of erysipelas.
- Non-invasive imaging techniques, like ultrasound and MRI, aid in visualizing skin and soft tissue involvement, guiding treatment decisions.
New Antimicrobial Agents
- Research is ongoing to develop new antibiotics with improved efficacy against Erysipelothrix rhusiopathiae, including macrolides, lincosamides, and fluoroquinolones.
- Combination therapies involving multiple antibiotics are being investigated to enhance antimicrobial activity and prevent resistance.
Immunotherapies
- Immunotherapies, such as monoclonal antibodies and cytokine modulators, are being explored to boost the host immune response against Erysipelothrix rhusiopathiae.
- These therapies aim to stimulate antibody production, enhance phagocytosis, and regulate inflammatory responses.
Surgical Interventions
- In severe cases of erysipelas, surgical debridement may be necessary to remove necrotic tissue and facilitate healing.
- Plastic surgery techniques are sometimes employed to reconstruct damaged skin and restore function.
Challenges and Future Directions
Despite advancements, challenges remain in erysipelas research. These include:
- Antimicrobial resistance is an emerging concern, necessitating the development of novel therapeutic strategies.
- Further research is needed to optimize diagnostic techniques for early detection and accurate identification of Erysipelothrix rhusiopathiae.
Future research directions include:
- Exploring the role of the microbiome in erysipelas pathogenesis and treatment.
- Developing personalized treatment approaches based on individual patient characteristics and risk factors.
Patient Education and Resources
Erysipelas, a bacterial skin infection, can be managed effectively with proper care and knowledge. Here’s a comprehensive guide to help you understand the condition, its treatment, and preventive measures.
Knowing the symptoms, treatment options, and preventive measures for erysipelas empowers you to take an active role in your health. This section provides valuable resources to help you navigate the condition effectively.
Symptoms
- Redness, warmth, and swelling of the affected skin
- Pain and tenderness
- Fever and chills
- Swollen lymph nodes
li>Blisters or ulcers
Treatment
- Antibiotics: The primary treatment for erysipelas is antibiotics, which are effective in eliminating the bacterial infection.
- Elevation and Rest: Elevating the affected limb and resting it can help reduce swelling and pain.
- Moisturizers: Keeping the affected area moisturized can help soothe the skin and prevent dryness.
- Compression: Applying gentle compression to the affected area can help reduce swelling.
- Pain Relievers: Over-the-counter pain relievers can help alleviate discomfort.
Prevention
- Good Hygiene: Practicing good hygiene, including washing hands frequently and keeping wounds clean, can help prevent infection.
- Skin Protection: Wearing protective clothing and using insect repellent can help prevent insect bites and scratches, which can lead to infection.
- Manage Underlying Conditions: If you have underlying conditions that weaken your immune system, such as diabetes or lymphedema, managing these conditions can help reduce your risk of developing erysipelas.
Support Resources, Erisipela
- Healthcare Providers: Consult with your doctor or healthcare provider if you suspect you have erysipelas. They can provide proper diagnosis and treatment.
- Patient Support Groups: Joining support groups can connect you with others who have experienced erysipelas, providing emotional support and sharing valuable insights.
- Online Resources: Reputable websites and online forums offer reliable information and support for patients with erysipelas.
Closing Summary
And there you have it, folks! Erisipela, a skin infection that can pack a punch, but with the right knowledge and treatment, it’s a foe you can conquer. Remember, prevention is key, so keep your skin clean, protected, and healthy. If Erisipela does come knocking, don’t panic! Seek medical attention promptly, follow your doctor’s orders, and watch this fiery invader retreat. Stay tuned for more health adventures, where we’ll tackle other intriguing medical mysteries!