Brain worms, a topic often shrouded in mystery, can have profound neurological effects on individuals. In this article, we delve into the complexities of brain worm infections, examining their neurological consequences, diagnosis, treatment options, and preventive measures.
From headaches and seizures to paralysis and cognitive impairment, brain worms can cause a range of neurological symptoms. Understanding the long-term effects of these infections, including brain damage, stroke, and dementia, is crucial for effective management and patient care.
Neurological Effects
Brain worms, parasitic flatworms that infest the central nervous system, can cause severe neurological damage. Their presence in the brain can lead to a range of symptoms, from headaches to seizures and paralysis.
Symptoms of Brain Worm Infestation
The symptoms of a brain worm infestation can vary depending on the location and severity of the infection. Common symptoms include:
- Headaches
- Seizures
- Paralysis
- Cognitive impairment
Long-Term Neurological Damage
If left untreated, brain worm infestations can cause permanent neurological damage. The worms can damage brain tissue, leading to:
- Brain damage
- Stroke
- Dementia
Parasitology
Brain worms are parasitic worms that can infect the brain and spinal cord of humans and animals. There are several different types of brain worms that can infect humans, each with its own unique life cycle and epidemiology.
Types of Brain Worms
- Taenia solium (pork tapeworm)
- Taenia saginata (beef tapeworm)
- Echinococcus granulosus (hydatid worm)
- Echinococcus multilocularis (alveolar echinococcosis)
- Angiostrongylus cantonensis (rat lungworm)
Life Cycle of Brain Worms
The life cycle of brain worms varies depending on the species of worm. However, in general, the life cycle involves the following steps:
- Eggs are passed in the feces of an infected host.
- Eggs are ingested by an intermediate host, such as a pig or cow.
- In the intermediate host, the eggs develop into larvae.
- Larvae migrate to the brain or spinal cord of the intermediate host.
- In the brain or spinal cord, the larvae develop into adult worms.
- Adult worms produce eggs, which are passed in the feces of the infected host.
Epidemiology of Brain Worm Infections
Brain worm infections are found worldwide, but they are most common in developing countries. The risk of infection is highest in areas where people live in close contact with animals, such as in rural areas or in areas where there is poor sanitation.
The most common type of brain worm infection in humans is caused by the pork tapeworm, Taenia solium. This infection is found in all parts of the world, but it is most common in Asia, Africa, and Latin America.
Diagnosis and Treatment
Diagnosing and treating brain worm infections requires a multifaceted approach involving various methods and treatment options. Accurate diagnosis is crucial for determining the appropriate course of treatment, which may include medications, surgery, or a combination of both.
Diagnostic Methods
- Neurological Examination: A physical exam assesses the patient’s neurological function, including motor skills, reflexes, and sensory perception, to detect any abnormalities caused by the infection.
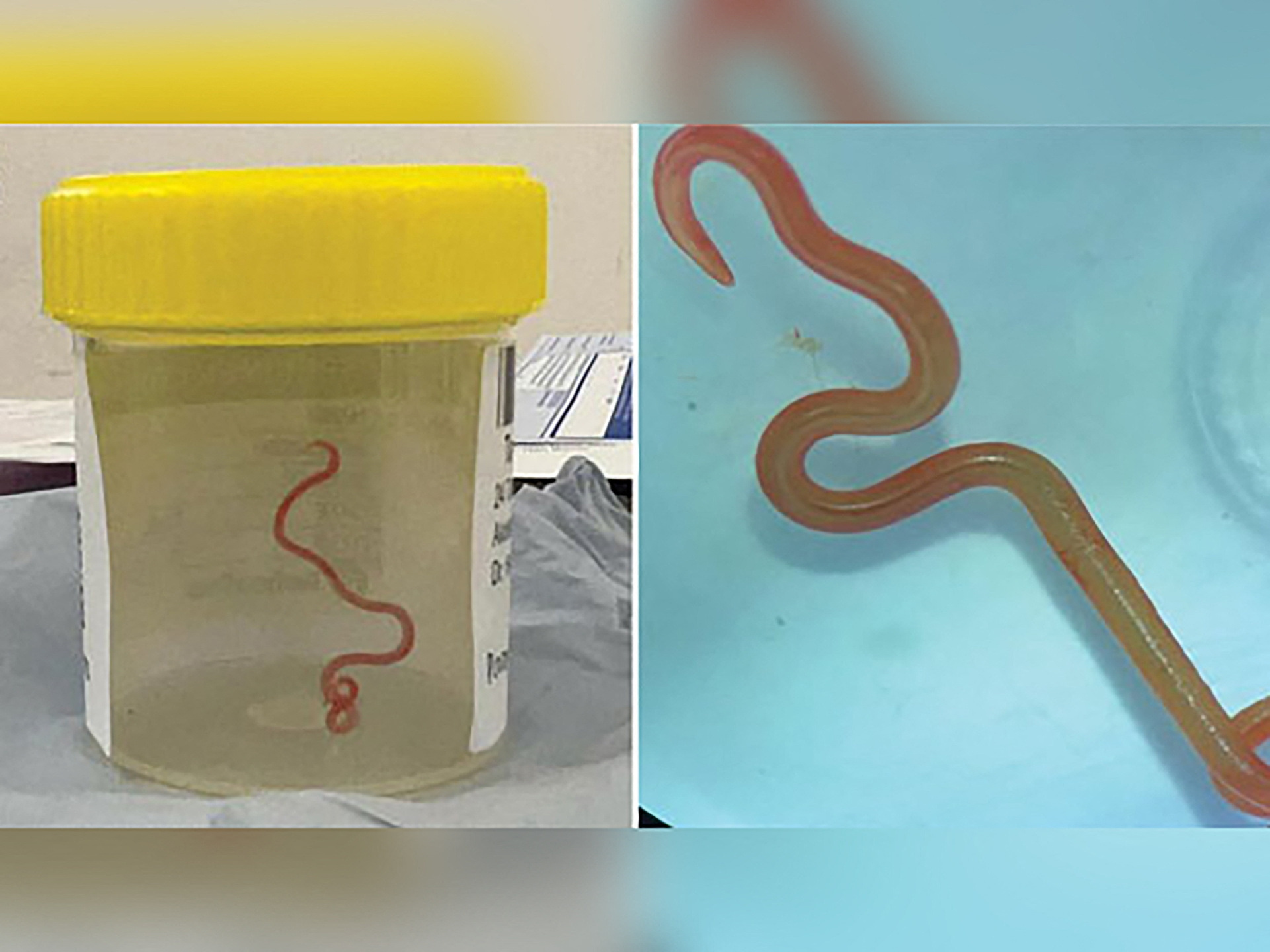
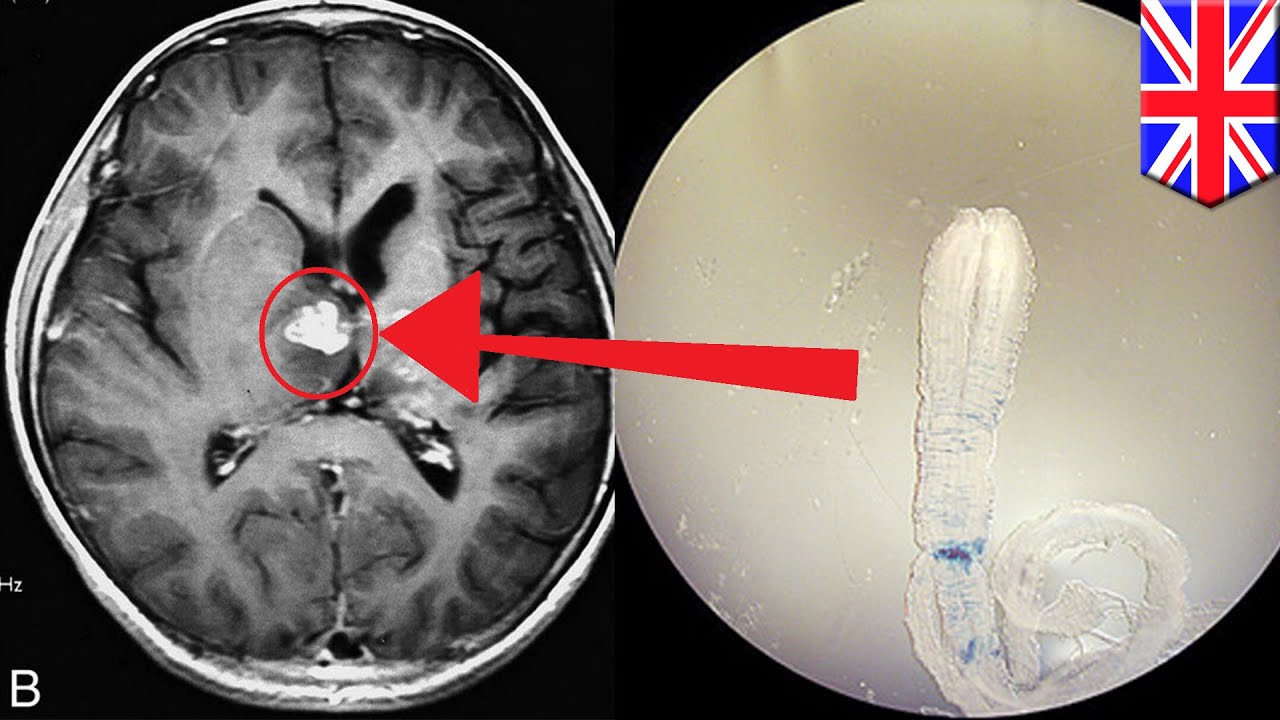
- Imaging Techniques: Magnetic resonance imaging (MRI) and computed tomography (CT) scans provide detailed images of the brain, allowing doctors to visualize any lesions or structural changes caused by the worms.
- Blood Tests: Blood samples can be tested for the presence of antibodies against the worm or its antigens, indicating an active infection.
- Cerebrospinal Fluid Analysis: A sample of cerebrospinal fluid, which surrounds the brain and spinal cord, can be examined for the presence of the worm or its eggs, confirming the diagnosis.
Treatment Options
- Antiparasitic Medications: Medications like albendazole and ivermectin are effective in killing brain worms. Treatment duration and dosage depend on the severity of the infection and the patient’s response.
- Surgery: In severe cases where medications fail or the infection is causing significant neurological damage, surgery may be necessary to remove the worms or relieve pressure on the brain.
Prognosis
The prognosis for patients with brain worm infections depends on several factors, including the severity of the infection, the timeliness of diagnosis and treatment, and the patient’s overall health. Early diagnosis and prompt treatment can significantly improve outcomes and prevent long-term complications.
Treatment Plan for a Patient with Brain Worm Infection
A treatment plan for a patient with a brain worm infection typically involves:
- Medication Regimen: A course of antiparasitic medication, such as albendazole, prescribed for a specific duration and dosage based on the patient’s condition.
- Follow-up Appointments: Regular follow-up appointments to monitor the patient’s progress, adjust medication as needed, and assess for any complications.
- Monitoring for Complications: Close monitoring for potential complications, such as seizures, increased intracranial pressure, or neurological deficits, and prompt intervention if necessary.
Prevention and Control
Brain worm infections can be prevented by practicing good hygiene, avoiding contact with contaminated water or soil, and using protective gear when working in areas with potential brain worm exposure. Public health measures such as surveillance, education, and sanitation programs also play a crucial role in controlling brain worm infections.
Proper Hygiene
Maintaining proper hygiene is essential in preventing brain worm infections. Wash your hands thoroughly with soap and water after coming into contact with animals or soil, especially in areas where brain worm infections are common. Avoid touching your face, especially your eyes and mouth, with unwashed hands.
Avoiding Contaminated Water and Soil
Brain worms can be transmitted through contact with contaminated water or soil. Avoid swimming or wading in water that may be contaminated with animal waste, such as ponds, lakes, or streams. Wear gloves and boots when working in areas with potential brain worm exposure, such as gardens or farms.
Protective Gear
When working in areas with potential brain worm exposure, wear protective gear such as gloves, boots, and a hat. This will help prevent contact with contaminated soil or water and reduce the risk of infection.
Case Studies
Case studies offer valuable insights into the clinical presentation, diagnosis, and treatment of brain worm infections. They provide real-world examples of how these infections manifest and the challenges faced by healthcare professionals in managing them.
Analyzing case studies helps identify common patterns, variations in clinical presentations, and effective treatment strategies. These lessons contribute to improving diagnostic accuracy, optimizing treatment approaches, and developing preventive measures.
Case Study Report
Patient Demographics
- Age: 35 years old
- Gender: Male
- Occupation: Farmer
Clinical Presentation
- Headache
- Nausea and vomiting
- Confusion
- Seizures
Diagnostic Tests
- Blood tests: Elevated eosinophil count
- Imaging studies (CT or MRI): Lesions in the brain
- Lumbar puncture: Elevated cerebrospinal fluid eosinophils
Treatment
- Antiparasitic medication (e.g., albendazole)
- Steroids to reduce inflammation
- Anticonvulsants to control seizures
Follow-up
- Symptoms resolved within 2 weeks of treatment
- Repeat imaging studies showed no residual lesions
- Patient remained asymptomatic during 1-year follow-up
This case study highlights the importance of considering brain worm infection in patients with eosinophilia and neurological symptoms, particularly in areas where these infections are endemic. Early diagnosis and prompt treatment can lead to a favorable outcome.
Historical Perspectives

The history of brain worms dates back to ancient times, with evidence of infections found in fossilized skulls. In the 16th century, Paracelsus, a Swiss physician, described brain worms as the cause of epilepsy. In the 17th century, the Dutch scientist Antonie van Leeuwenhoek discovered the first brain worm, a nematode parasite.
Early Physicians and Scientists
In the 18th and 19th centuries, scientists began to study brain worms in more detail. The German physician Rudolf Virchow identified the pork tapeworm as a cause of brain worm infections. The French scientist Jean-Baptiste Charcot described the symptoms of brain worm infections, including seizures, headaches, and personality changes.
Cultural and Societal Implications
Brain worm infections have had a significant impact on cultures and societies throughout history. In some cultures, brain worms were believed to be caused by evil spirits or witchcraft. In other cultures, brain worms were seen as a sign of divine punishment. Today, brain worm infections are still a serious public health problem in many parts of the world.
Comparative Parasitology
Brain worms belong to a diverse group of parasitic organisms that infect the nervous system. They share certain similarities and differences with other parasites that target the brain and spinal cord.
Life Cycles
The life cycles of brain worms vary depending on the species. Some, like Angiostrongylus cantonensis, have complex life cycles involving multiple hosts, including snails, rodents, and humans. Others, like Gnathostoma spinigerum, have simpler life cycles with only one intermediate host.
Symptoms
The symptoms of brain worm infections can range from mild to severe. Common symptoms include headaches, nausea, vomiting, seizures, and neurological deficits. The severity of symptoms depends on the parasite species, the number of worms present, and the location of the infection.
Treatment
The treatment for brain worm infections typically involves antiparasitic medications. These medications can be effective in killing the worms and reducing symptoms. However, treatment may be challenging if the infection is severe or if the worms have spread to the brain.
Evolutionary Relationships
Brain worms are believed to have evolved from free-living nematodes. Over time, they have adapted to survive and reproduce within the nervous system of their hosts. The evolutionary relationships between brain worms and other parasites are still being studied, but it is clear that they share a common ancestry.
Pathophysiology: Brain Worms
Brain worm infections are caused by parasitic worms that migrate to the brain and cause neurological damage. The lifecycle of the parasite involves ingestion of eggs, which hatch into larvae in the intestine. The larvae then migrate through the bloodstream to the brain, where they mature into adult worms. The adult worms can live in the brain for many years, causing chronic inflammation and damage.
The mechanisms by which brain worms cause neurological damage are not fully understood, but they are thought to involve a combination of tissue invasion, inflammation, and immune-mediated damage. The worms can invade brain tissue, causing direct damage to neurons and other brain cells. They can also trigger an inflammatory response, which can lead to further damage to brain tissue. Additionally, the immune system can mount an attack against the worms, which can also cause damage to brain tissue.
The immune response to brain worm infections is complex and involves both innate and adaptive immunity. Innate immunity is the body’s first line of defense against infection and involves the activation of cells such as macrophages and neutrophils. Adaptive immunity is a more specific response that involves the activation of T cells and B cells. Both innate and adaptive immunity are important for controlling brain worm infections, but they can also contribute to the neurological damage that is caused by the infection.
The following table summarizes the key findings of research on the pathophysiology of brain worm infections:
| Finding | Mechanism | Consequences |
|—|—|—|
| Tissue invasion | Direct damage to neurons and other brain cells | Neurological damage |
| Inflammation | Release of inflammatory cytokines | Swelling and damage to brain tissue |
| Immune-mediated damage | Attack by T cells and B cells | Further damage to brain tissue |
The pathophysiology of brain worm infections leads to a variety of clinical manifestations, including seizures, headaches, nausea, vomiting, and changes in behavior. The severity of the clinical manifestations depends on the number of worms in the brain, the location of the worms, and the host’s immune response.
Neuroimaging
Neuroimaging plays a crucial role in diagnosing and monitoring brain worm infections. By visualizing the brain and its structures, neuroimaging techniques help identify the presence, location, and extent of brain worm infestations.
Computed Tomography (CT)
- CT scans provide detailed cross-sectional images of the brain, allowing visualization of brain worm cysts or lesions.
- CT is particularly useful for detecting calcified brain worm cysts, which appear as dense, well-defined structures.
Magnetic Resonance Imaging (MRI)
- MRI offers high-resolution images of the brain, providing detailed information about brain worm morphology and tissue damage.
- MRI can detect both cystic and parenchymal brain worm lesions, as well as associated inflammation and edema.
Diffusion Tensor Imaging (DTI)
- DTI measures the diffusion of water molecules in the brain, providing insights into the integrity of white matter tracts.
- In brain worm infections, DTI can detect abnormalities in white matter connectivity, indicating damage to neural pathways.
Neuroimaging Findings in Brain Worm Infections
Neuroimaging findings associated with brain worm infections vary depending on the parasite species, infection stage, and host response. Common findings include:
- Cysts or lesions in the brain parenchyma, ventricles, or subarachnoid space
- Enhancing lesions on contrast-enhanced MRI, indicating active inflammation
- Edema and mass effect, causing increased intracranial pressure
- White matter abnormalities, including reduced fractional anisotropy on DTI
Molecular Biology

Brain worms, also known as Angiostrongylus cantonensis, are parasitic nematodes that can infect the brain and spinal cord of humans and other animals. The molecular biology of brain worms is complex and involves a variety of genes and proteins that are essential for their development and pathogenesis.
Genome, Transcriptome, and Proteome
The genome of A. cantonensis has been sequenced and analyzed, revealing a complex genetic makeup with a large number of genes. The transcriptome and proteome of brain worms have also been studied, providing insights into the gene expression and protein profiles that are associated with different stages of their life cycle and pathogenic mechanisms.
Genes and Proteins Involved in Development and Pathogenesis
Numerous genes and proteins have been identified that play key roles in the development and pathogenesis of brain worms. These include genes involved in:
- Larval migration and invasion of the central nervous system
- Establishment of infection in the brain and spinal cord
- Immune evasion and modulation
- Tissue damage and inflammation
The expression patterns and functions of these genes and proteins are currently being investigated, with the aim of identifying potential molecular targets for the treatment of brain worm infections.
Potential for Molecular Targets
The molecular biology of brain worms offers promising opportunities for the development of new and effective treatments. Potential molecular targets include:
- Genes and proteins essential for larval migration and invasion
- Molecules involved in immune evasion and modulation
- Proteins responsible for tissue damage and inflammation
By targeting these molecules, it may be possible to develop drugs, vaccines, and diagnostic markers that can effectively prevent and treat brain worm infections.
Current State of Research
Research on molecular targets for brain worm infections is still in its early stages, but there has been significant progress in recent years. Several potential targets have been identified, and some promising drug candidates are currently being evaluated in preclinical studies.
Future Directions, Brain worms
Future research on molecular targets for brain worm infections should focus on:
- Validating potential targets and identifying their mechanisms of action
- Developing new drug candidates and evaluating their efficacy and safety
- Exploring the potential for combination therapies
- Investigating the molecular basis of drug resistance
By continuing to investigate the molecular biology of brain worms, we can improve our understanding of these parasites and develop more effective strategies for their control and treatment.
Finish your research with information from Frosinone ‘Inter.
Potential for Molecular Targets for the Treatment of Brain Worm Infections
Molecular targets for the treatment of brain worm infections are promising due to their potential for specificity and efficacy. However, further research is needed to identify and validate these targets.
Biochemistry
Brain worm infections induce a cascade of biochemical alterations that profoundly impact the host’s neurological function. These worms secrete an array of bioactive molecules that disrupt the delicate metabolic balance within the brain.
Metabolic Pathways Affected
Brain worms manipulate host metabolism to sustain their own growth and survival. They primarily target glucose metabolism, diverting glucose from the host’s energy production pathways to fuel their own energy demands. Additionally, they disrupt lipid and amino acid metabolism, leading to imbalances in essential nutrients and neurotransmitters.
Potential for Biochemical Interventions
Understanding the biochemical mechanisms underlying brain worm infections presents potential avenues for therapeutic intervention. By targeting specific metabolic pathways exploited by the worms, researchers aim to develop drugs that inhibit their growth and survival. Such interventions could provide novel and effective treatments for these debilitating infections.
– Discuss the global distribution and prevalence of brain worm infections.

Brain worm infections are a major public health concern in many parts of the world. The most common brain worm infection is caused by the parasite Angiostrongylus cantonensis, which is found in Southeast Asia, the Pacific Islands, and parts of the Americas. Other brain worm infections, such as those caused by Baylisascaris procyonis and Gnathostoma spinigerum, are found in different parts of the world.
You also can investigate more thoroughly about Marica Pellegrinelli to enhance your awareness in the field of Marica Pellegrinelli.
The prevalence of brain worm infections varies depending on the region and the specific parasite. In some areas, such as Southeast Asia, the prevalence of A. cantonensis infection can be as high as 50%. In other areas, such as the United States, the prevalence of brain worm infections is much lower.
Research Directions

Ongoing research in the field of brain worm infections is driven by the need to enhance our understanding of these parasites, improve diagnostic techniques, and develop more effective treatment and prevention strategies. Current research directions include:
Emerging Technologies and Methodologies
- Molecular diagnostics: Advancements in molecular biology have led to the development of highly sensitive and specific diagnostic tests for brain worm infections, such as PCR (polymerase chain reaction) and LAMP (loop-mediated isothermal amplification).
- Imaging techniques: Advanced imaging techniques, such as MRI (magnetic resonance imaging) and CT (computed tomography), provide detailed images of the brain and can aid in the diagnosis and monitoring of brain worm infections.
- Bioinformatics: Bioinformatics tools are used to analyze large datasets generated from genomic and transcriptomic studies of brain worms, providing insights into their biology and potential targets for intervention.
Future Advancements
Future research directions are expected to focus on:
- Development of new drugs and therapies: The development of new drugs and therapies is crucial for the effective treatment of brain worm infections. Research efforts are focused on identifying novel targets for drug development and exploring alternative treatment strategies, such as immunotherapies.
- Improved prevention and control measures: Enhanced surveillance and monitoring systems are essential for preventing and controlling brain worm infections. Research is ongoing to develop effective vector control measures and improve sanitation practices in endemic areas.
- Understanding the long-term effects of brain worm infections: Long-term studies are needed to assess the impact of brain worm infections on cognitive function, behavior, and overall health. This knowledge will inform the development of appropriate rehabilitation and support programs for individuals affected by these infections.
Concluding Remarks
Brain worm infections, while potentially severe, can be effectively diagnosed and treated with proper medical care. By raising awareness about the risks and implementing preventive measures, we can significantly reduce the burden of brain worm infections and improve the overall health and well-being of individuals.