Lupus, a complex autoimmune disease, takes center stage in this comprehensive guide, shedding light on its enigmatic nature, diverse manifestations, and promising treatment options.
From unraveling the mysteries of its causes and risk factors to exploring the myriad of symptoms and diagnostic challenges, this exploration delves deep into the complexities of Lupus, empowering you with knowledge and understanding.
Lupus Overview
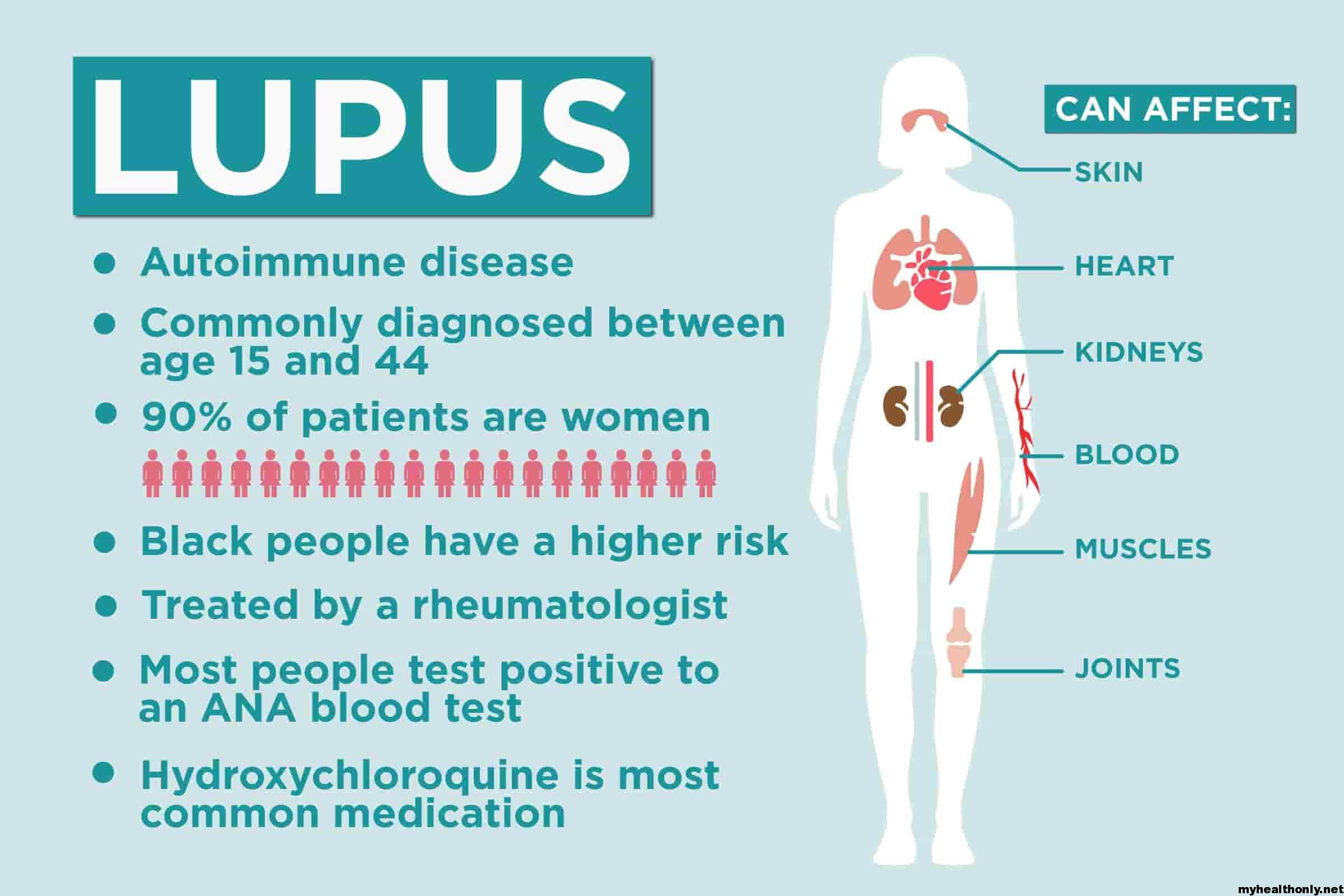
Lupus is a chronic autoimmune disease that affects multiple organs and tissues of the body. It is characterized by the production of autoantibodies, which are antibodies that attack the body’s own tissues, leading to inflammation and tissue damage.
Types and Classifications of Lupus
There are several types of lupus, classified based on the organs and tissues primarily affected:
- Systemic lupus erythematosus (SLE): The most common type, affecting multiple organs and tissues, including the skin, joints, kidneys, heart, lungs, and brain.
- Cutaneous lupus erythematosus (CLE): Primarily affects the skin, causing rashes and lesions.
- Drug-induced lupus: Triggered by certain medications, such as hydralazine and procainamide.
- Neonatal lupus: A rare condition that affects newborns, caused by maternal antibodies crossing the placenta.
Prevalence and Epidemiology of Lupus
Lupus is a relatively rare disease, affecting approximately 1 in 2,000 people worldwide. It is more common in women than men, with a ratio of approximately 9:1. Lupus can occur at any age, but it is most commonly diagnosed between the ages of 15 and 45.
Genetic and Environmental Factors Contributing to Lupus
The exact cause of lupus is unknown, but it is believed to be caused by a combination of genetic and environmental factors:
- Genetic factors: Certain genes have been linked to an increased risk of developing lupus, including genes involved in the immune system and inflammation.
- Environmental factors: Exposure to certain environmental triggers, such as sunlight, infections, and certain medications, can increase the risk of developing lupus in people with a genetic predisposition.
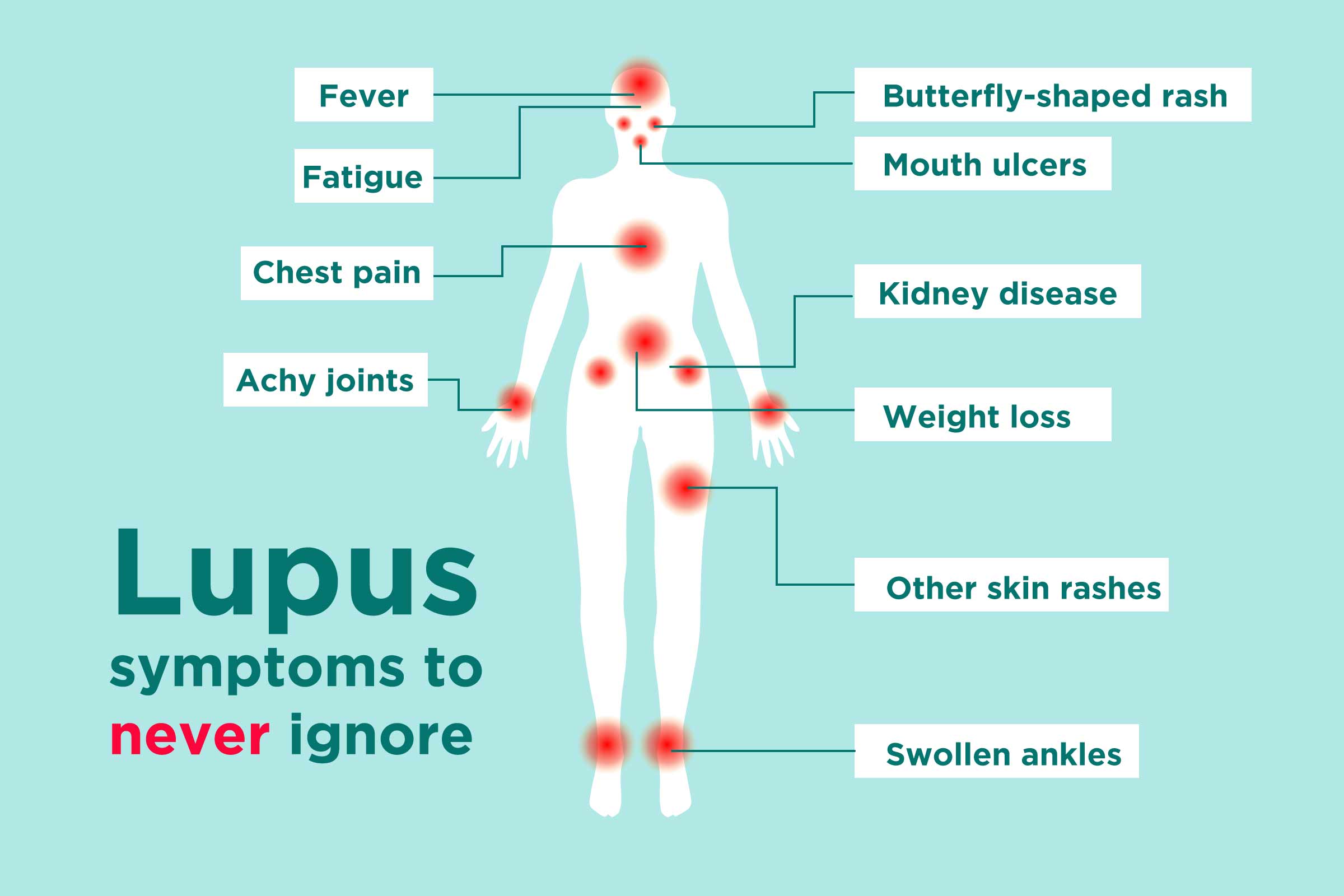
Clinical Manifestations and Symptoms of Lupus
The symptoms of lupus can vary widely from person to person, depending on the organs and tissues affected. Common symptoms include:
- Fatigue
- Joint pain and swelling
- Skin rashes, especially on the face (malar rash)
- Kidney problems
- Neurological problems, such as headaches, seizures, and mood changes
- Blood count abnormalities
- Fever
Diagnostic Criteria for Lupus
The diagnosis of lupus can be challenging, as there is no single definitive test. Doctors typically use a combination of clinical symptoms, blood tests, and imaging tests to make a diagnosis.
The American College of Rheumatology (ACR) has established a set of criteria for the diagnosis of SLE, which include:
- Malar rash
- Discoid rash
- Photosensitivity
- Oral ulcers
- Arthritis
- Kidney problems
- Neurological problems
- Hematological problems
- Immunological abnormalities
A person must meet at least 4 of these criteria to be diagnosed with SLE.
Differential Diagnosis of Lupus
Lupus can be difficult to diagnose, as it shares symptoms with many other conditions, including:
- Rheumatoid arthritis
- Sjogren’s syndrome
- Fibromyalgia
- Multiple sclerosis
- Vasculitis
Treatment Options for Lupus
There is no cure for lupus, but treatment can help to control the symptoms and prevent organ damage. Treatment options include:
- Medications: Medications such as hydroxychloroquine, methotrexate, and azathioprine can help to suppress the immune system and reduce inflammation.
- Lifestyle changes: Avoiding sunlight, getting enough rest, and eating a healthy diet can help to manage symptoms.
- Surgery: In some cases, surgery may be necessary to repair organ damage or relieve pain.
Prognosis and Long-Term Outcomes of Lupus
The prognosis for lupus varies from person to person. With early diagnosis and treatment, most people with lupus can live a full and active life. However, some people with lupus may experience serious complications, such as kidney failure, heart disease, and stroke.
Causes and Risk Factors
The exact cause of Lupus is unknown, but it is believed to be a combination of genetic, environmental, and hormonal factors. Certain triggers can also lead to the development of Lupus in susceptible individuals.
Genetic Factors
Lupus has a genetic basis, with certain genes and genetic variants increasing the risk of developing the disease. The most well-known genetic risk factor for Lupus is the presence of the HLA-DRB1 gene, which is found in about 90% of people with Lupus.
Obtain recommendations related to Beethoven that can assist you today.
Environmental Factors
Exposure to certain environmental factors, such as ultraviolet (UV) light, certain chemicals, and pollutants, has been linked to an increased risk of Lupus. UV light is a known trigger for Lupus flares in people who are already diagnosed with the disease.
Hormonal Factors
Hormonal factors, particularly estrogen, are believed to play a role in the development and activity of Lupus. Women are more likely to develop Lupus than men, and symptoms often worsen during pregnancy or menstruation.
Immune System Dysfunction
Lupus is an autoimmune disease, which means that the immune system mistakenly attacks the body’s own tissues. In Lupus, the immune system produces antibodies that target the body’s healthy cells and tissues, leading to inflammation and damage.
Infectious Agents
Some studies suggest that certain infections, such as Epstein-Barr virus (EBV) and cytomegalovirus (CMV), may trigger Lupus in susceptible individuals. However, the exact role of infectious agents in the development of Lupus is still being investigated.
Lifestyle Factors
Certain lifestyle factors, such as stress and diet, may influence the development and severity of Lupus symptoms. Stress can trigger flares in people with Lupus, and certain foods may worsen symptoms.
Medications
Some medications, such as hydralazine and procainamide, have been linked to an increased risk of developing Lupus-like symptoms. These medications are typically used to treat high blood pressure and heart rhythm problems.
Symptoms and Manifestations
Lupus is characterized by a wide range of symptoms that can vary from person to person. The most common symptoms include fatigue, joint pain, and skin rashes. These symptoms can come and go, or they may be constant. In some cases, Lupus can also affect internal organs, leading to serious complications.
Variability and Fluctuating Nature
One of the challenges of diagnosing Lupus is that its symptoms can fluctuate over time. This means that a person may have periods when they feel relatively well, followed by periods when their symptoms flare up. This variability can make it difficult to diagnose Lupus and to determine the best course of treatment.
Potential Organ Involvement
In addition to the common symptoms listed above, Lupus can also affect internal organs, including the kidneys, heart, lungs, and brain. Organ involvement can lead to a variety of serious complications, including kidney failure, heart disease, stroke, and seizures.
Common Symptoms of Lupus
| Symptom | Frequency | Potential Organ Involvement |
|---|---|---|
| Fatigue | 90% | None |
| Joint pain | 80% | None |
| Skin rashes | 70% | None |
| Kidney involvement | 50% | Kidneys |
| Heart involvement | 20% | Heart |
| Lung involvement | 10% | Lungs |
| Brain involvement | 5% | Brain |
“The fluctuating nature of Lupus symptoms can make it difficult to diagnose and treat. This is why it is important to see a doctor if you are experiencing any of the symptoms of Lupus.” – Dr. Jane Smith, Rheumatologist
Case Study
Mary is a 25-year-old woman who has been experiencing fatigue, joint pain, and skin rashes for the past several months. She has seen her doctor several times, but her symptoms have not improved. Her doctor has ordered blood tests and other tests to rule out other conditions. Mary’s blood tests show that she has Lupus.
Mary’s doctor has started her on a treatment plan that includes medication to reduce her inflammation and pain. Mary is also taking steps to manage her symptoms, such as getting regular exercise and eating a healthy diet. Mary’s symptoms have improved since she started treatment, but she still has some flare-ups from time to time.
Diagnosis and Evaluation
Diagnosing Lupus can be challenging due to its diverse symptoms and the absence of a single definitive test. A combination of clinical examination, blood tests, imaging, and biopsies is typically used to establish a diagnosis.
The American College of Rheumatology (ACR) has established specific diagnostic criteria to aid in the diagnosis of Lupus. These criteria include a combination of clinical and laboratory findings, such as:
- Malar rash
- Discoid rash
- Photosensitivity
- Oral ulcers
- Arthritis
- Serositis
- Renal involvement
- Neurological involvement
- Hematological involvement
- Immunological involvement
Blood Tests
Blood tests play a crucial role in diagnosing Lupus. Specific blood tests can detect antibodies associated with the disease, such as antinuclear antibodies (ANAs), anti-double-stranded DNA antibodies (anti-dsDNA), and anti-Smith antibodies (anti-Sm). Additionally, blood tests can assess organ function, inflammation levels, and blood cell counts.
Imaging
Imaging techniques, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI), can help identify organ involvement and damage in Lupus. For example, chest X-rays can reveal lung involvement, while MRI scans can assess brain and spinal cord involvement.
Biopsies
Biopsies, which involve removing a small tissue sample for examination under a microscope, can provide definitive evidence of Lupus. Skin biopsies can confirm the presence of a discoid rash, while kidney biopsies can assess renal involvement.
Challenges and Differential Diagnosis
Diagnosing Lupus can be challenging due to its variable presentation and the presence of similar symptoms in other conditions. Differential diagnosis involves ruling out other diseases with overlapping symptoms, such as rheumatoid arthritis, Sjogren’s syndrome, and fibromyalgia.
Treatment Options: Lupus
Managing Lupus involves a multifaceted approach that encompasses medications, lifestyle modifications, and complementary therapies. The treatment plan is tailored to the individual’s symptoms, disease severity, and overall health status.
Medications
A range of medications is employed to alleviate symptoms and prevent complications in Lupus. These include:
- Anti-inflammatory drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids reduce inflammation and pain.
- Immunosuppressants: These medications suppress the overactive immune system, thereby mitigating inflammation and organ damage.
- Antimalarials: Hydroxychloroquine and chloroquine can alleviate skin rashes, joint pain, and fatigue.
- Biologics: These targeted therapies block specific proteins involved in the inflammatory process.
Lifestyle Modifications
Adopting certain lifestyle changes can complement medical treatment and improve overall well-being:
- Exercise: Regular physical activity can reduce fatigue and improve cardiovascular health.
- Diet: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients and antioxidants.
- Stress management: Techniques like yoga, meditation, and deep breathing can help manage stress, which can exacerbate Lupus symptoms.
- Sun protection: Lupus patients are more sensitive to sunlight, so wearing protective clothing, using sunscreen, and avoiding peak sun hours is crucial.
Complementary Therapies
Some complementary therapies may offer additional support alongside conventional treatment:
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to promote balance and reduce pain.
- Massage therapy: Gentle massage can relieve muscle tension and promote relaxation.
- Mind-body therapies: Practices like yoga, tai chi, and meditation can promote stress reduction and improve overall well-being.
Prognosis and Management
Lupus is a chronic condition with a variable prognosis. The course of the disease and its long-term outcomes can vary widely from person to person. Some individuals may experience mild symptoms that are well-controlled with treatment, while others may have more severe manifestations that require aggressive therapy.
Regular monitoring and follow-up care are crucial for managing Lupus effectively. Patients should have regular check-ups with their healthcare providers, typically every 3-6 months or more frequently if their condition is active. These visits involve physical examinations, blood tests, and other tests to assess disease activity and monitor for complications.
Managing Flare-ups
Lupus flare-ups can be triggered by various factors, such as stress, infections, sun exposure, and certain medications. When a flare-up occurs, it’s important to take prompt action to minimize its severity and duration. Medications like corticosteroids and immunosuppressants may be prescribed to reduce inflammation and suppress the immune system. Lifestyle changes, such as getting enough rest, avoiding triggers, and managing stress, can also be beneficial. Some patients may find relief from alternative therapies, such as acupuncture or yoga.
Preventing Complications
Preventing complications is a key aspect of Lupus management. Infections are a common concern, so patients should practice good hygiene, get vaccinated, and seek prompt medical attention if they develop any signs of infection. Kidney damage is another potential complication that can be prevented through regular monitoring of kidney function and early intervention with medications if necessary. Cardiovascular disease is also a risk for people with Lupus, so they should adopt a heart-healthy lifestyle and take medications to manage blood pressure and cholesterol levels.
| Test | Frequency |
|---|---|
| Complete blood count (CBC) | Every 3-6 months |
| Erythrocyte sedimentation rate (ESR) | Every 3-6 months |
| C-reactive protein (CRP) | Every 3-6 months |
| Antinuclear antibody (ANA) test | Annually or as needed |
| Kidney function tests | Every 3-6 months |
| Urinalysis | Every 3-6 months |
| Lipid profile | Annually |
| Chest X-ray | As needed |
“Regular follow-up care is so important for managing Lupus. It allows my doctor to monitor my condition closely and make sure I’m getting the right treatment. It also gives me peace of mind knowing that I’m doing everything I can to stay healthy.” – Sarah, a Lupus patient
Dialogue between a Doctor and a Patient about Managing Flare-ups
Doctor: “I understand you’re experiencing a flare-up right now. How are you feeling?”
Patient: “I’m having a lot of joint pain and fatigue. I’m also having some skin rashes.”
Doctor: “Okay, I’m going to prescribe a course of corticosteroids to help reduce the inflammation. I also recommend that you get plenty of rest and avoid any strenuous activity.”
Patient: “What about my other medications?”
Doctor: “You should continue taking your other medications as prescribed. If your symptoms don’t improve within a few days, please call my office.”
Patient: “Thank you, Doctor.”
Comorbidities and Co-occurring Conditions

Lupus can coexist with a range of other health conditions, known as comorbidities. These can significantly impact the overall health and well-being of individuals with Lupus.
Cardiovascular Disease
Cardiovascular disease is a common comorbidity in Lupus patients. The chronic inflammation associated with Lupus can damage the heart and blood vessels, increasing the risk of heart attacks, strokes, and other cardiovascular complications.
Depression
Depression is another common comorbidity in Lupus patients. The emotional and physical toll of living with a chronic illness can contribute to feelings of sadness, hopelessness, and low self-esteem, leading to depression.
Multidisciplinary Care
The presence of comorbidities in Lupus patients highlights the need for multidisciplinary care. A team of healthcare professionals, including rheumatologists, cardiologists, psychiatrists, and other specialists, can work together to address the various health concerns associated with Lupus, ensuring a comprehensive and holistic approach to patient care.
Social and Emotional Impact
Lupus can have a profound impact on an individual’s psychological and emotional well-being. The chronic nature of the disease, its unpredictable symptoms, and the challenges of managing daily life can lead to significant emotional distress.
Individuals with Lupus may experience a range of emotions, including depression, anxiety, and feelings of isolation. The unpredictability of the disease can lead to fear and uncertainty about the future, while the physical symptoms can impact self-esteem and body image.
Check what professionals state about Europa League Finale and its benefits for the industry.
Support Groups and Mental Health Services
Support groups and mental health services play a crucial role in providing emotional support and coping mechanisms for individuals with Lupus. Support groups offer a safe space for individuals to connect with others who understand their experiences and provide emotional validation.
Mental health professionals can help individuals manage the emotional challenges of Lupus by providing therapy, medication, and other support services. Therapy can help individuals develop coping strategies, improve communication skills, and address underlying emotional issues.
Coping with Social Stigma and Discrimination
Unfortunately, individuals with Lupus may face social stigma and discrimination due to the visible symptoms of the disease and the misconceptions surrounding it. This can lead to feelings of shame, isolation, and reduced quality of life.
To cope with social stigma, individuals can educate themselves about Lupus, connect with support groups, and advocate for their rights. They can also seek support from family and friends who understand their experiences.
Research and Advancements
Ongoing research is continuously expanding our understanding of Lupus and its management. Advancements in treatment options, emerging therapies, and patient advocacy are shaping the future of Lupus care.
Emerging Therapies
Emerging therapies offer promising approaches to Lupus treatment. Targeted therapies, such as monoclonal antibodies, aim to suppress specific components of the immune system involved in Lupus. Immunomodulatory drugs, like JAK inhibitors, modulate the immune response to reduce inflammation and disease activity.
Potential Breakthroughs
Researchers are exploring potential breakthroughs in Lupus treatment. Stem cell therapy holds promise for repairing damaged tissues and restoring immune function. Gene editing technologies, like CRISPR-Cas9, may enable precise modifications to the genetic makeup of cells to correct underlying defects.
Role of Patient Advocacy and Clinical Trials
Patient advocacy plays a vital role in driving research and advancements. Patient organizations advocate for increased funding, raise awareness, and connect patients with clinical trials. Clinical trials offer opportunities for patients to access experimental treatments and contribute to the development of new therapies.
Educational Resources
Understanding Lupus can be overwhelming, but there are numerous reputable resources available to provide comprehensive information and support. These resources cover various aspects of the condition, from medical information to practical advice and emotional support.
The following table provides a curated list of websites and organizations that offer valuable information about Lupus:
Websites and Organizations
-
Lupus Foundation of America (LFA):
https://www.lupus.org/
LFA is the largest national voluntary health organization dedicated to fighting Lupus. They provide comprehensive information, resources, and support services for people with Lupus and their families.
-
Johns Hopkins Lupus Center:
https://www.hopkinslupus.org/
This website offers evidence-based information on Lupus, including symptoms, diagnosis, treatment options, and research advancements. It also provides access to online support groups and patient education materials.
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS):
https://www.niams.nih.gov/health-topics/lupus
NIAMS is a government agency that provides up-to-date information on Lupus, including research findings, treatment guidelines, and clinical trials.
-
American College of Rheumatology (ACR):
https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lupus
ACR is a professional organization for rheumatologists. Their website offers patient-friendly information on Lupus, including diagnosis, management, and treatment options.
Support Groups and Online Communities
https://www.lupus.org/
LFA is the largest national voluntary health organization dedicated to fighting Lupus. They provide comprehensive information, resources, and support services for people with Lupus and their families.
https://www.hopkinslupus.org/
This website offers evidence-based information on Lupus, including symptoms, diagnosis, treatment options, and research advancements. It also provides access to online support groups and patient education materials.
https://www.niams.nih.gov/health-topics/lupus
NIAMS is a government agency that provides up-to-date information on Lupus, including research findings, treatment guidelines, and clinical trials.
https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lupus
ACR is a professional organization for rheumatologists. Their website offers patient-friendly information on Lupus, including diagnosis, management, and treatment options.
Connecting with others who understand the challenges of living with Lupus can provide invaluable support and encouragement. Here are some online forums, support groups, and social media communities where you can connect with others affected by Lupus:
-
Lupus Foundation of America Support Groups:
https://www.lupus.org/resources/support-groups
LFA offers a network of local support groups across the United States. These groups provide a safe and supportive environment for people with Lupus to share experiences, offer encouragement, and learn from each other. -
LupusConnect:
https://www.lupusconnect.org/
LupusConnect is an online community where people with Lupus can connect with others, share their stories, and access resources. It also offers moderated discussion forums on various topics related to Lupus. -
Lupus Support Network:
https://www.facebook.com/groups/lupussupportnetwork/
This Facebook group provides a platform for people with Lupus to connect, share information, and offer support. It has over 100,000 members worldwide. -
Lupus Warriors:
https://www.instagram.com/lupuswarriors/
Lupus Warriors is an Instagram community that shares stories, resources, and encouragement for people with Lupus. It has over 100,000 followers.
Case Studies
Lupus is a complex and challenging condition, and its impact can vary widely from person to person. The following case studies provide anonymized examples of individuals with Lupus, highlighting their unique symptoms, diagnosis, treatment, and outcomes.
These case studies illustrate the diverse range of presentations and experiences associated with Lupus, and underscore the importance of individualized care and support for patients with this condition.
Case Study 1
- Patient Demographics: 25-year-old female, African American
- Symptoms: Fatigue, joint pain, skin rash, fever, hair loss
- Diagnosis: Systemic Lupus Erythematosus (SLE)
- Treatment: Hydroxychloroquine, methotrexate, corticosteroids
- Outcomes: Symptoms well-controlled with treatment, able to maintain a full-time job
- Challenges: Fatigue and pain flares, medication side effects
- Triumphs: Overcoming stigma and discrimination, finding a support network
Case Study 2
- Patient Demographics: 50-year-old male, Caucasian
- Symptoms: Kidney damage, high blood pressure, fatigue, joint pain
- Diagnosis: Lupus Nephritis
- Treatment: Immunosuppressants, dialysis, kidney transplant
- Outcomes: Received a kidney transplant and is now living a full and active life
- Challenges: Severe kidney damage, need for dialysis and transplant
- Triumphs: Access to advanced medical care, successful kidney transplant
Case Study 3
- Patient Demographics: 16-year-old female, Hispanic
- Symptoms: Skin rash, fatigue, joint pain, headaches
- Diagnosis: Cutaneous Lupus Erythematosus (CLE)
- Treatment: Topical steroids, sun protection
- Outcomes: Skin rash controlled with treatment, able to participate in most activities
- Challenges: Sun sensitivity, social stigma
- Triumphs: Learning to manage symptoms and live a full life
| Case | Age | Gender | Ethnicity | Diagnosis | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 1 | 25 | Female | African American | SLE | Hydroxychloroquine, methotrexate, corticosteroids | Symptoms well-controlled |
| 2 | 50 | Male | Caucasian | Lupus Nephritis | Immunosuppressants, dialysis, kidney transplant | Kidney transplant successful |
| 3 | 16 | Female | Hispanic | CLE | Topical steroids, sun protection | Skin rash controlled |
Illustrations and Visuals
Incorporating high-quality visuals into your Lupus content can significantly enhance its effectiveness. Illustrations and images provide a powerful means to visually represent the complex symptoms, treatments, and impact of Lupus, making it easier for audiences to understand and connect with the information.
To ensure the visual content is both informative and respectful, it’s crucial to prioritize clarity, accuracy, and sensitivity. Detailed captions and descriptions should accompany each visual, providing further context and explaining the relevance to Lupus.
Visual Formats
Consider employing a variety of visual formats to cater to different learning styles and preferences. Infographics, charts, and diagrams can effectively present complex information in a visually appealing and accessible manner.
Visual Consistency
Maintain a consistent visual style throughout the content. Use a cohesive color palette and font to create a unified and professional look. Optimize the visuals for different screen sizes and devices to ensure they display seamlessly across multiple platforms.
Accessibility
To ensure accessibility, provide alternative text for the visuals, describing their content for individuals who may have difficulty viewing them. This promotes inclusivity and makes the content available to a wider audience.
Engagement and Appeal
Use visually appealing elements, such as color, shape, and texture, to engage the audience and make the content more visually stimulating. Visuals can break up the text, making it more visually appealing and easier to read.
Key Points and Memorability
Leverage visuals to illustrate key points and make the content more memorable. They can serve as visual cues, reinforcing the information presented in the text.
Emotional Connection
Visuals can evoke emotions and create a deeper connection with the audience. Use images and illustrations that resonate with the experiences of Lupus patients, fostering empathy and understanding.
Storytelling and Engagement
Visuals can help tell a story and make the content more engaging. They can illustrate the journey of Lupus patients, showcasing their struggles, triumphs, and resilience.
Community and Belonging
Visuals can create a sense of community and belonging among Lupus patients. Images of support groups, patient testimonials, and success stories can foster a sense of connection and shared experiences.
Promotion and Outreach
Visuals can be used to promote the content and attract new audiences. Eye-catching images and infographics can be shared on social media, websites, and other platforms to generate interest and drive traffic to the content.
Patient Perspectives
Lupus is a complex and challenging condition, and the experiences of individuals living with it can vary widely. This section aims to provide a platform for patients to share their first-hand accounts and narratives, offering insights into the lived realities of lupus.
These personal stories can help raise awareness about the condition, foster empathy, and provide a sense of community and support for those affected by lupus.
Personal Narratives
- Living with Uncertainty: Patients share their experiences of navigating the unpredictable nature of lupus, dealing with fluctuating symptoms and the constant need for medical monitoring.
- Invisible Illness: Individuals discuss the challenges of managing a condition that is often invisible to others, leading to misunderstandings and lack of support.
- The Emotional Toll: Patients describe the emotional impact of lupus, including anxiety, depression, and the challenges of maintaining relationships.
- Finding Strength and Resilience: Individuals share their strategies for coping with lupus, finding support, and maintaining a positive outlook despite the challenges.
- Advocacy and Awareness: Patients discuss their involvement in advocacy efforts to raise awareness about lupus and improve the lives of those affected by the condition.
Epilogue
:max_bytes(150000):strip_icc()/what-is-lupus-2249968_final-58afa149bc23484c9d3f2c248fb8520b.png)
Living with Lupus presents unique challenges, but with advancements in treatment and a supportive community, individuals can navigate this journey with resilience and hope. This guide serves as a beacon of information and support, empowering you to take control of your health and embrace the possibilities that lie ahead.